Its 5:30 am. I roll over and swipe right to my COVID tracker and news feeds; India, Brazil and Mexico continue to surge, with cases in the US and Europe spiking – in some cases to new heights – across states and countries each day. Northern Ireland halts and delays any further lockdown easing as the now infamous R0 number rises across the population.
All this to say, the future of the COVID-19 crisis is by no means certain, recent warnings from the WHO’s Director General, Dr Tedros Adhanom Ghebreyesus, emphasising the very real fact that, across the globe, “the pandemic is still accelerating”. Where we had previously begun to see a trend in countries taking the reigns over the spread of their outbreaks, recent weeks have shown worrying resurgences of COVID-19 in countries where the situation had been thought to be improving. Headlines and breaking news alerts have seen the US appear as a recurring figure amidst growing concerns over the global crisis, daily cases now spiking over the 60,000 mark and well above any figures seen in the country during its assumed initial wave. Meanwhile, many states continue to re-open businesses, and a not insignificant proportion of the population refuse to wear masks or adhere to general social distancing rules. Undoubtedly, the degree of community spread has surged over these recent weeks, and with it comes fear that the country is not far away from a reality where daily cases reach 100,000, should nothing be done to rectify a worsening spiral out of control.
With the constant barrage of news around resurging outbreaks across the globe, I get asked this question several times a day and countless times each week – “When is the second wave coming, and how severe will it be?”. As we all know, an exact science for the date, time and precise volume of cases or mortalities would be challenging for the best of us. However, for me, the question behind that question is “what do we need to do to be ready, insulated and more?”. We know from the first wave that of the over 2 million patients shielding in the UK, the majority were indeed protected from the virus. We also know that strong lockdown strategies worked well. What we have no experience of is COVID-19 combined with the complexities of winter, flu season, as well as an economy which is likely to return to previous levels of lockdown, and the impact this blend would have on the country’s R0, case numbers, peak volumes and mortality rate. What we do know is that there will be a number of mini spikes over the coming months and an eventual second wave, and so we look to answering the big question – “What will this really look like?
Before writing, the team told me “Orlando, don’t plug D&D in your article”. Well, here is the plug. Our predictive solutions – used across the NHS and even as far as Abu Dhabi at leading health provider SEHA, in collaboration with John Hopkins, both in acute and mental health settings – were fundamental during the first wave and are currently being used in rapid recovery, tactical and strategic planning. To learn more about the how, please feel free to reach out on LinkedIn or directly through our website. And now, back to the article.
As health systems and technology-based firms such as our own continue to examine the wealth of data generated over the course of the pandemic, a crucial consideration is how the pandemic has affected mortality rates over this time, and what this may imply for future waves. Although death rates above previous years’ averages will have been expected as a result of COVID-19, what is perhaps even more concerning is the rise in non-COVID deaths over this time, peaking within the UK in correlation with the height of the pandemic. While excess deaths in both have since fallen in-line with the impact of social distancing and lockdown measures, this trend in non-COVID mortality will be a serious consideration in the weeks to come.
The lack of capacity to treat patients arriving at hospitals already overwhelmed with the sheer volume of COVID-19 patients has been one of the biggest fears across the NHS since the virus first began to build momentum. In the wake of the pandemic, this has since been even further compounded by difficulties around patients experiencing symptoms of cancer, stroke and cardiovascular issues forgoing trips to potential COVID-19 hotbeds, as well as the cancellation of non-urgent procedures over this period. It is clear that, if we are to avoid similar spikes in excess deaths during a secondary wave, measures must be put in place now in order to ensure we do not see a subsequent wave of avoidable deaths as a result of capacity issues and inefficient services.
A Future Outlook: Predicting the Second Wave

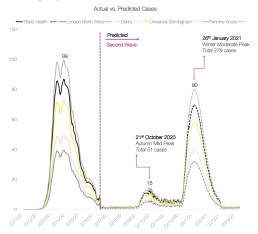
Throughout even the early days of China’s epidemic and as initial reports of a novel coronavirus began to emerge, we have worked around the clock to generate the predictions and supporting solutions vital to ensuring trusts are fully prepared for the extreme exacerbation of a pre-existing demand-capacity issue across the NHS. As the threat of a second wave looms, further developing our predictions to shed light on what may be in store over the coming months and year has been a true focal point of our work as a company, integrating the UK’s COVID-19 journey so far with deep level research and analysis of the global situation, particularly in those countries further ahead of our own growth trajectory.
Indeed, while the resurgence of a second COVID-19 wave appears to inevitable, it is likely that these future waves will not hit the same peaks in case volumes seen at the outbreak’s height in late April. Nonetheless, in the context of a national health service already on the brink of full capacity and a workforce buffeted by an onslaught of constant pressures, this spike in cases and the resulting translation to surging patient numbers highlights an urgent need to ensure trusts will be able to handle the oncoming caseload, building from this knowledge of when and to what extent the country may see a renewed influx of potentially critically ill patients in order to redirect and secure sufficient resources to cope with increasing demand.


The severity and impact of COVID-19 has certainly not been uniform across the country or between trusts, and we have seen regions such as London and the South East hit more severely than others over the course of the pandemic. Trust-specific predictions, particularly for those who experienced the highest number of deaths during the initial outbreak, have therefore formed a significant part of our ongoing second wave work, incorporating the individual caseloads already seen at each with our own researched assumptions and proprietary algorithms. By supporting each trust in better understanding what their future COVID-19 situation may look like, it is my honest belief that we will be able to ensure the necessary bed capacity, resource availability, and workforce strength essential to protecting patients in the face of one of the most significant global events in living history.
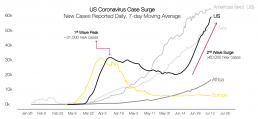
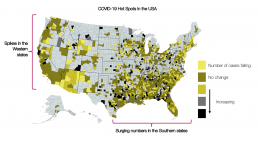
Looking back to the US’s current worsening COVID-19 landscape, it is clear that even within the country, notable hotspots have been seen across the Southern and Western states, likely owing to the individual response policies employed by each region and the resulting disparities in effectively controlling any continued spread. With the similarities to the UK’s own regional differences in both COVID-19 caseloads and overall mortality rates, it is vital that we begin planning for a secondary wave in-line with that of the US across our own shores, establishing which regions have experienced the greatest impact from COVID-19 thus far, and how this may reflect upon their situation following the onset of a second wave. While the hope remains that any upsurge in new cases across the UK does not reach the same levels seen during the first wave of the pandemic, much of this will rely upon how the country handles a return to “business as usual” and the reopening of public spaces to minimise spread, as well as how our NHS organisations are able to prepare for oncoming pressures upon healthcare and workforce capacity. What is clear is that the current situation in the US is a stark reminder of what may be in store for the UK should we not take proactive steps in guaranteeing we have planned and fully equipped ourselves – and the first step to doing so is ensuring we know what to expect, and when.
The UK’s COVID-19 Situation
Already, the virus has reached over 13.3m individuals across the globe, killing at least 578k so far and doubling over the past 6 weeks. With more than half of these cases having been reported within the Americas alone, it is clear that this is not an issue of national wealth, both high and low economic countries having fared poorly in the wake of the pandemic. What has been a crucial component of success in countries that have achieved good control over their outbreaks is a strong starting position in terms of their health systems, combined with more intensive public health measures, such as broad testing, tracing and isolation of those who have been exposed. Establishing these corner stones of a successful COVID-19 response has seen countries even with more modest means maintain effective management of the virus’s impact, much of this involving a strategy that initiated pro-active steps before the pandemic had even reached their borders.
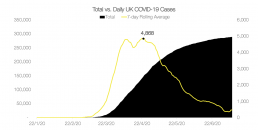
With this comes an important lesson for the UK – groundwork for the next wave must begin now if we are to ensure our health systems are adequately prepared and our patients fully protected. We have seemingly passed our first COVID-19 peak, but with this comes its own challenges. Once again, people have begun to return to the outside world; schools welcoming their students back to classrooms, pubs and restaurants reopening their doors to patrons, and many patients who had attempted to avoid exposure during the height of the pandemic now beginning to seek medical attention for issues they may have previously been ignoring. It is a necessary step, many argue, to restart businesses and the economy after months of lockdown, and that refusing to do so will bring more harm than good to the country. However, it is undeniable that with increased social interaction will come an eventual surge in new cases as we continue to operate in the absence of a COVID-19 vaccine.
Indeed, while we began with the recent ominous statement from the WHO’s Director General, we similarly end with a sentiment from Dr Tedros that I truly support as we head into second wave and recovery planning – “the virus can be brought under control”. With the right resources, support and preparation, I am confident that healthcare systems both across the UK and the globe will be able to combine the pro-active response capabilities enabled by our predictive solutions with the strong leadership essential to implementing them within hospitals, ensuring that our patients are able to receive the care they desperately need in the oncoming crisis. For those of you who wish to learn more about our predictive solutions and second wave planning, please visit us at our website, email us at info@draperanddash.com, or message me here on LinkedIn.