Reducing surgical backlogs and harm in a second surge by Orlando Agrippa, CEO, Draper & Dash
5 years, 10 million, burnout, avalanche of harm. These are the words which many of my senior colleagues across health systems have been using as part of their growing concerns as to where healthcare currently is. A great number say it will take five years to even get our mojo back to basic levels of delivering healthcare, and another five years to properly recover. Countless others are also predicting a staggering growth in waiting lists as the tip of the iceberg, significant harm to patients sitting just beneath the surface, in a surge to 10 million patients backlogged by Christmas.In a round table discussion with a number of Chief Executives and Medical Directors, concern over the welfare of our healthcare workforce was consistently a key priority amongst healthcare leadership – many already seeing large numbers of staff off sick with increasing levels of anxiety, back pains, and more. In an environment of vast and pre-existing strain due to an already scarce workforce, this is a real issue for all.
So where are we now?
Each week the waiting lists surge. Greater and greater numbers of patients face ongoing pain and worry as they await their chance to undergo surgery for procedures categorised as non-urgent, and as the pandemic continues to rage on – edging towards a full-blown secondary wave in the UK and across the globe – it is likely that these patients will be forced to continue waiting over the coming months, others joining them in this limbo as time goes on. From strained bed, operating theatre, and workforce capacities to cancellations in the hopes of reducing the risk of exposure to the virus, pre-existing surgical backlogs have only been further exacerbated by the pandemic, and exist as a substantial concern among healthcare providers across the board as we now move towards the Winter months.
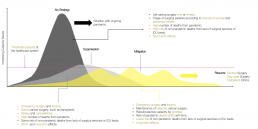
The number of patients waiting more than 52 weeks for treatment has sky-rocketed over the past year, soaring from 3,097 in March of 2020 to 111,026 patients as of August 2020 – a 3,584% increase in just 5 months. With each additional weekly or monthly delay in treatment, patients face the significant risk of further deterioration in their physical and psychological wellbeing. Without urgent and intensive action, many of these patients will see deferrals that take them to, and even over, the tipping point of irreversible damage, and we will begin to see increasing numbers of patients saddled with the permanent yet indirect impact of the pandemic. As the risk of preventable patient harm and mortality grows, it is clear that measures need to be taken now to reduce and subvert the negative consequences an emerging second wave and oncoming flu season, as well as the ongoing demand surge, may have on already strained services.
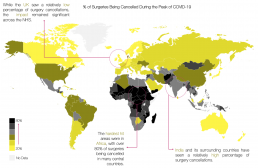
While this impact on surgical backlogs across the NHS has been notable, it is certainly not an issue restricted at a national level. Across the globe, countries have struggled to maintain normal services and support patients in need of non-urgent surgical procedures, with the US alone seeing millions deferred in an attempt to halt the spread of the virus and reserve a level of capacity for rising influxes of critically ill patients. Though elective care has since resumed, following the first peak of the pandemic, local surges in caseloads have seen an inconsistent pattern of care as services were paused to limit further spread. Indeed, as the UK and others see similar patterns of localised outbreaks and soaring R0 numbers, the need to address the ongoing strategy in tackling the pandemic at both an organisational and national level is a prominent one, and it will be vital for healthcare providers to deploy whatever tools are afforded by current technological advancements, in order to ensure systems aren’t overwhelmed and that patients aren’t left to suffer because of it.
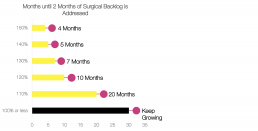
Already, organisations have begun to look into potential means of resolving these issues, with a central focus involving the need to ensure facilities work above the levels of efficiency achieved during previous years in order to begin the process of cutting backlogs. Early analysis has identified the need to work to at least 110% of previous years’ functionality in order to prevent further growth of these backlogs as demand continues to surge – improvement even to this level still seeing a 20-month period before a 2-month surgical backlog could be cleared. To support in successfully providing treatment to these deferred patients, healthcare organisations have already begun to establish action plans at both a near-term and medium-term level, much of this focusing around evaluating operating room block allocations and extending hours of operation, in addition to contacting patients in order to limit cancellations.
While an important first phase in the strategic process, it will be crucial to further support providers, healthcare workers, and teams on the ground in reaching these substantially increased levels of activity and efficiency through the deployment of advanced technological and data science solutions. Reducing the manual burden of analytics and response modelling, as well as arming users with the predictive insight essential to fully preparing organisations in light of the approaching second wave, these solutions therefore strive to:
1. Reduce any unnecessary deferral of care.
2. Address new challenges to throughput in an effective and more automated manner.
3. Forecast upcoming demand to a higher degree of accuracy, and balancing the necessary capacity to match this in real-time.
4. Extend this into a longer-term increase in provider capacities to ensure sustained improvements, by reimagining operating room procedures.
Already, we (Draper & Dash) have been working in the background throughout the pandemic – and in the face of a second wave and demand surge – to ensure healthcare teams are equipped with the advanced analytics and AI/ML tools needed to truly deliver on effectively managing waiting lists and surgical care backlogs. While many have followed news cycles and fresh reports of increasing delays to treatment with growing concern, deploying our Health Data Science Platform (DSP) at one partner organisation has already demonstrated a clear benefit in supporting forward planning across the trust – establishing the strategies needed to ensure the strong management of restarted elective services and deferred patients at a short, medium, and long-term level. Particularly in light of increasing respiratory disease-related activity as we enter the Winter period of combined COVID-19 and seasonal influenza, the trust was in need of a data-driven approach to driving both this short-term and longer-term recovery plan, in order to address climbing elective waiting lists, with additional high-level planning and business case design to support the creation of a new hospital to tackle demand.
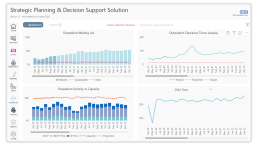
As a result, our DSP was selected in order to tackle these central challenges, modelling surge and capacity beyond a localised and setting-orientated level, and to the financial and workforce recovery planning needed across key situations within the hospital environment. Covering the breadth of services from emergency department, outpatient and inpatient utilisation, the DSP worked to forecast demand across the entire realm of settings and services at the trust – 10 years into the future. By combining this with COVID-19 specific projections at a range of best to worst case scenarios, based upon specifics in timing and severity, the trust has therefore been able to model the impact of the pandemic and beyond in terms of the capacity needed to fully handle and prevent the overwhelming of its services.
Leveraging these insights and predictive capabilities through the response modelling functionality of the DSP further allowed the trust to test and model the effectiveness of potential strategies and their resulting impact, prior to deployment, ensuring the true impact of any responses could be fully visualised and any alterations needed to deliver optimised approaches could be shaped. Arming users with the power to build these potential response strategies by adjusting in-depth parameters such as new or redirected capacity, shifted site-by-site demand, or operational efficiency measures including patient lengths of stay or daycase procedures, the DSP’s advanced modelling techniques, interconnected methodology, and stringent logic translated to key operational, financial, capacity, and efficiency impacts. Through this, strategic planning was supported at every level, allowing the trust to adequately prepare for impending surges and review the flow of patients throughout the system – tackling surgical and elective backlogs in an environment where many healthcare providers continue to struggle under staggering pressures.