By Orlando Agrippa, CEO, Draper & Dash.
In a matter of weeks, we have catapulted into a typhoon of planning, reconfiguring capacity, building field hospitals, and scrambling for Personal Protective Equipment (PPE), as we continue to fight one of the deadliest viruses of our time. Panting, as teams keel over from the first wave, they immediately gather themselves and push on to the next furlong to recovery and the second phase.
In a recent closed discussion with several provider and system level Chief Operating Officers (COOs), Chief Finance Officers (CFOs) and recovery directors, we discussed modelling the impact of all planning assumptions in real time, alongside recovery programme support, featured at the top of the urgent priority list. Some of the highlights discussed were:
- Ascertain the upcoming demand
- Establish the resulting capacity needed
- Begin work on assessing the delivery models and clinical pathways, down to specialty level, in those that may be especially fragile or vulnerable such as cardiology, neurology, gastroenterology, and ENT
- Ensuring a collective view across care boundaries
- Detailing a route map from a modelling system perspective, such as to identify patients who may now have an altered risk profile, due to their underlying comorbidities and the heightened vulnerability to the virus that these may present.
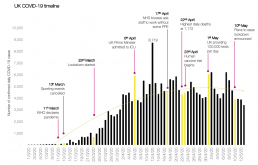
For all of us, this is new stuff; the assumptions we need to make about cancer patients, green sites, fragility cohorting, predicting demand and impact, shielding patients, the impact on PPE packs, and system working. You name it. Modelling hundreds of scenarios to ensure we get this right is a challenge for so many. This, when compounded with the arrival of seasonal flu in five months’ time, leaves us with a lot to be done in a very short window. A true race and test of endurance, strategy, resilience, and system working.
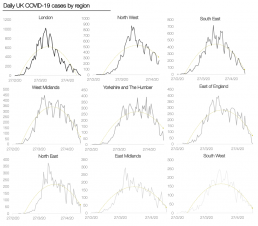
More and more focus across the country now looks to the easing of lockdown restrictions, a return to what many consider to be the “new normal” as we start to show signs of cresting the COVID-19 peak. Following in the footsteps of the countries ahead of us on COVID-19’s outbreak curve, our handling of an emergence from lockdown will ultimately rely on our actions today. And so, the biggest questions at a fundamental level for healthcare organisations planning around a post-lockdown ecosystem revolve around this – what might we need to deliver, and how will we do it?
Mapping the constraints to recovery planning
Lockdown has left a population raring to venture back into the outside world, and while most have avoided trips to their GP or A&E over recent months out of fear of the virus and to reduce the already heavy burden on our doctors and nurses, I can only imagine that we are about to see a surge in attendances across healthcare organisations. As elective procedures begin again and new patients start to arrive, the need for PPE in treating a population that has yet to see COVID-19 completely eradicated will only become more important in minimising a resurgence of the pandemic.
Sites performing high volumes of elective work, particularly procedures such as endoscopies and tonsillectomies which require around 40 and 10 pieces of PPE per procedure, respectively, may face an even greater struggle to secure adequate protection for their workforce. Ensuring that we model these constraints accurately in the face of an unknown supply chain will be a crucial component of any recovery planning, in order to guarantee sound management of upcoming and future theatre lists and work plans.
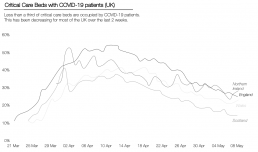
Venturing a layer down from this issue lies the resulting impact on our healthcare workforce, all of whom have been hit hard with the exhaustion of battling COVID-19 over the past months. Coupling an estimated 16% sickness rate with the usual yearly sickness absences, it is clear that any trust in the process of recovery planning will need to factor this substantial constraint in modelling their ongoing capacity. Healthcare workers are some of the most at risk of infection in the face of COVID-19, and having already been diminished in number by shielding, 7–14 day self-isolation, and even positive re-tests despite being asymptomatic, we are likely to see a significant blow to the very healthcare teams essential to handling the upcoming wave of post-COVID-19 activity.

Alongside this stands the issue of diagnostic constraints. Touching back on an issue that has been at the heart of a lot of Draper & Dash’s solutions over the years, the flow of elective work will be determined at a top level by the availability of PPE, as well as by the wait time for diagnostics. In the context of COVID-19, staff at many trusts currently undergo a long journey in returning to work following a positive diagnosis. After the 7 to 14-day isolation period, a second test is usually performed, equating to an additional 2-day wait, and followed by CT scanning. Numerous trusts already face vast limitations in terms of their CT capacity, and with the added burden of scans needed in the diagnosis of COVID-19, this will only be exacerbated in the coming months.
The impact of limitations to PPE, diagnostics, and the subsequent effect on workforce capacity will be vital considerations as recovery planning takes place. While known components of this process, modelling of what these constraints will actually look like in order to effectively manage demand and capacity remains an ongoing issue.
Tackling the demand vs. capacity divide
As we move through the initial stages of modelling key constraints and applying this to recovery planning, what lies at the heart of these efforts will be an investigation of the demand gap and establishing how to best serve that gap. In doing so, it will be crucial to ensure that providers are still working to guarantee that safe and high-quality outcomes are delivered, that patients are risk assessed efficiently, and that they are also able to optimise the capacity available. A significant part of this will be for providers to begin looking beyond organisation level planning and to consider capacity at a system level. Organisational recovery cannot feasibly be covered purely by operating locally, instead requiring work that stretches across the system so that, where capacity may be limited at one site, patients will still be able to receive treatment they need elsewhere.
Speaking with several NHS colleagues over recent weeks, the approach being taken by many trusts is firstly to ascertain the upcoming demand, secondly to establish the resulting capacity needed, and thirdly to begin work on assessing the delivery models and clinical pathways, down to specialty level, in those that may be especially fragile or vulnerable such as cardiology, neurology, gastroenterology, and ENT. While certainly not a feat to be taken lightly, I am confident that modelling at this level would be best served through the efforts of several teams creating individual project support pieces, eventually feeding into an overarching programme from which the system as a whole can excel.
Again, much of this has been structured around the need to blur the boundaries of an organisation as its own entity, focusing instead on ensuring each patient is treated as quickly as possible and as safely as possible. Some of the most promising progress I have encountered so far has come from working alongside collaborative efforts between multiple trusts and providers, gathering a collective view of what the key issues are in terms of demand and operational processes. From this, we have been able to look to the next phase of capacity planning at a system, subsystem, and provider level, establishing what the gap between demand and capacity will be in order to truly achieve organisational recovery.
From an initial role in scoping and collating the needs of our partner trusts, creating a detailed route map of what the future looks like, we therefore apply D&D’s extensive technological background to support modelling from a system perspective, combined with the project management expertise of our development team. In the current COVID-19 climate, an important component of this utilises the ability of our solution to identify patients who may now have an altered risk profile, due to their underlying comorbidities and the heightened vulnerability to the virus that these may present. Patients diagnosed particularly with the big 5 COVID-19 risk factors, such as diabetes and cardiovascular disease, who may initially have been assessed to be safe to receive an elective procedure, could now face a much higher and inappropriate degree of risk due to the possibility of coronavirus infection.
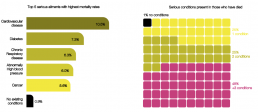
Any modelling will therefore need to take these altered risk profiles into consideration, balancing potential exposure to COVID-19 with the impact of delaying a procedure on quality of life and an established “tipping point”. In situations such as a patient waiting for a hip replacement or treatment for glaucoma, there will be a clinical point beyond which deterioration of the patient’s wellbeing will become irreversible and any future treatments will be less, if at all, effective. As such, D&D’s solution analyses and models these layers of complexity, in order to support clinicians and the healthcare team in identifying and reassessing patients who may need to delay treatment or be reprioritised in order to prevent harm.
With the ever-present concern of a second COVID-19 wave this Autumn in the absence of a vaccine, combined with the usual pressures of a seasonal flu, nothing matters more to us than to further support trusts looking to the future, building upon this initial modelling and recovery planning by incorporating an additional predictive element. Through this, our goal is to provide organisations with as powerful an arsenal as possible for ongoing preparations, ensuring our partners have as much time as possible to implement the necessary measures needed to protect their workforces and continue delivering high quality patient care in the face of the ongoing COVID-19 pandemic.
For anyone who wishes to learn more about our recovery planning support, we welcome you to reach out to us at info@draperanddash.com.