By Orlando Agrippa, CEO, Draper & Dash.
At the time of writing this article, 2020 moves further into a period we have not seen the likes of in living human history. With over 50,542 fatalities as a result of COVID-19 since the onset of the outbreak, this surge in mortality has compounded with the numbers already seen throughout the country prior to the pandemic – approximately 293,000 deaths from over 9.4 million recorded discharges, either while in hospital or within 30 days of discharge, for the 129 hospital trusts recorded. Now more than ever, the role of the Medical Examiner and the Structured Judgement Review (SJR) is essential. One can only imagine the demands on Medical Examiners across the country such as the National Chief Medical Examiner, Dr Alan Fletcher, and it is the duty of companies such as Draper & Dash to apply our technological capabilities to best help those working to improve the outcomes of our friends and loved ones every day.

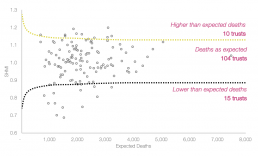
In the face of these mounting pressures, we have been steadfast in supporting our NHS colleagues in ensuring strong visibility and rigour around the mortality review process. Part of the current learning and recovery planning process for each trust has a foundation in the annual national mortality report, the most recent January-December 2019 release seeing 10 trusts, around 8% of those covered, with higher than expected mortalities. Within this, key diagnosis groups included pneumonia, septicaemia and acute congestive heart failure, these being of particularly significance in the context of COVID-19 due to pneumonia and sepsis comprising common complications of the virus in more severe cases, often resulting in mortality among these patients.
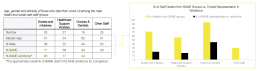
We have also seen some worrying patient demographic-based trends across our NHS trusts over the course of the pandemic, many reporting a significant disparity in the number of deaths seen between different ethnicities, both within our healthcare workforce and the population as a whole. In a matter of weeks, figures began to highlight the severe impact COVID-19 was having on BAME members of the NHS workforce, disproportionately high deaths rates seen in nurses, midwives, healthcare support workers, doctors, dentists, as well as other staff. Despite accounting for only around 21% of the workforce overall, BAME individuals comprised 63% of total COVID-19 staff deaths, highlighting a significant underlying issue that needs urgent addressing.
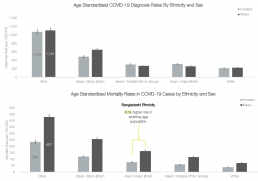
With BAME individuals further accounting for 34% of patients admitted to UK intensive care units with COVID-19, again despite comprising only 17% of the UK’s population, the government established an enquiry in order to attempt to identify the underlying reason for these glaring disparities. However, as of recent data released by Public Health England covering laboratory confirmed cases up to May 13th, these striking differences remained true, with death rates highest among black and Asian ethnic groups in a notable reversal from pre-COVID-19 trends, which saw higher deaths rates due to any cause amongst white ethnic groups. Even now, the reasons for this disparity have not been clearly established, whether it be due to biological and genetic reasons translating to greater susceptibility, due to medical reasons and associated comorbidities such as hypertension and diabetes, or due to sociological reasons and employment or working patterns that carry a higher risk of exposure and transmission. Ultimately, it is a question that needs answers fast, in order to ensure we can tackle these disparities and protect those who have now been widely seen to be an incredibly vulnerable group in the face of COVID-19.
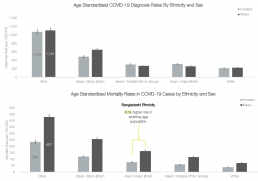
With BAME individuals further accounting for 34% of patients admitted to UK intensive care units with COVID-19, again despite comprising only 17% of the UK’s population, the government established an enquiry in order to attempt to identify the underlying reason for these glaring disparities. However, as of recent data released by Public Health England covering laboratory confirmed cases up to May 13th, these striking differences remained true, with death rates highest among black and Asian ethnic groups in a notable reversal from pre-COVID-19 trends, which saw higher deaths rates due to any cause amongst white ethnic groups. Even now, the reasons for this disparity have not been clearly established, whether it be due to biological and genetic reasons translating to greater susceptibility, due to medical reasons and associated comorbidities such as hypertension and diabetes, or due to sociological reasons and employment or working patterns that carry a higher risk of exposure and transmission. Ultimately, it is a question that needs answers fast, in order to ensure we can tackle these disparities and protect those who have now been widely seen to be an incredibly vulnerable group in the face of COVID-19.
Both pre-COVID-19 and into the ongoing pandemic, D&D’s goal has always been to support our NHS colleagues in ensuring optimal hospital management and high-quality patient outcomes. With the many issues and severe impact the virus has had on hospitals and their mortality rates, we have already begun to deploy the Clinical Outcomes Review System (CORS) across a number of NHS trusts, delivering some real improvements to date. Already, the CORS programme has been of unparalleled value to the SJRs, Medical Examiners (MEs), and attending physicians upon which so much of the learning and recovery process depends – some key outcomes of which I am delighted to be able to share with you now.
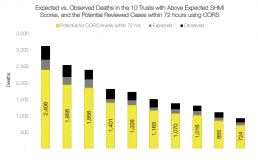
Within the trial sites already utilising CORS, healthcare teams have been able to review 100% of all tested patients with boosted COVID-19 surveillance monitoring, in addition to excellent turnaround times for the completion of Qualified Attending Physicians (QAP) reviews, 72% now completed within 72 hours of death. Similarly, ME reviews have seen an upsurge in turnaround time, now at 76% completion within 72 hours of death, with approximately 27 fewer consultant reviews now needed – from 35% to 13%. With SJR reviews now at 83% within 72 hours, the CORS programme has delivered more efficient management of mortality reviews, with significant efficiency savings for the clinical governance team. These savings have also been translated to the informatics teams, the overall improvements in efficiency to the mortality review and learning from deaths process allowing for real-time and automated outcome reporting.
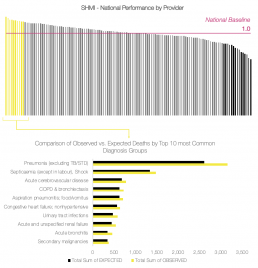
I am confident that by utilising CORS at those trusts reporting SHMI numbers above the national baseline, in particular those 10 with scores that are classified as higher than expected, we will soon be able to see similar improvements to mortality reviewing, learning, and subsequently the overall death rates at these trusts. With these 10 trusts collectively reporting 17,890 observed deaths over the January-December 2019 period, 2,495 over the expected number, the ability of CORS to boost efficiency by 77% on average across the QAP, ME and SJR processes could see around 13,775 of these observed patient deaths reviewed within 72 hours.
As we continue to fight the added burden of COVID-19 across the NHS, supporting clinical teams in accurately and efficiently reviewing each death to ensure the full learning potential is achieved will be truly crucial. It is my honest belief that programmes such as CORS will be essential components of securing this, and for those who those who are interested in learning more about the platform, we welcome you to reach out to us here or on our website at https://draperanddash.com/solutions-2/clinical-outcome-review-system/ or info@draperanddash.com